SAQ
Question 1
a) Outline the production and circulation of cerebrospinal fluid (CSF) and how intracranial pressure affects production and absorption. (5 marks)
b) How does the biochemistry of CSF differ from plasma? (4 marks)
c) List the indications for lumbar puncture. (6 marks)
d) Which factors predispose to the development of a post-dural puncture headache after lumbar puncture? (5 marks)
Question 2
You are asked to sedate a frightened adult patient for insertion of dental implants in an outpatient dental chair.
a) Complete the table in your answer booklet with the four levels of sedation in the American Society of Anesthesiologists (ASA) continuum of sedation (top row) and the clinical features seen at each level (columns below). (8 marks)
b) Outline drugs that may be used and their methods of administration, when providing sedation for this patient (4 marks)
c) What are the best practice principles for providing safe sedation to this patient? (8 marks)
Question 3
A 25 year-old woman who is 37 weeks pregnant and known to have pre-eclampsia is admitted to your labour ward with a blood pressure of 160/110mmHg on several readings.
a) What is the definition of pre-eclampsia (1 mark) and which related symptoms should pregnant women be told to report immediately? (2 marks)
b) How should this patient be managed following admission to your labour ward? (12 marks)
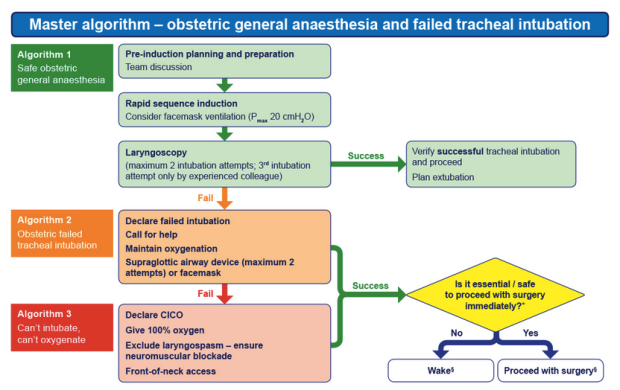
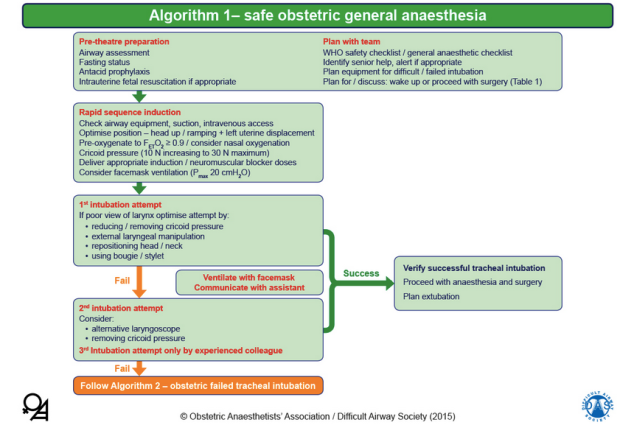
c) What changes would you make to your usual general anaesthetic technique for a pregnant woman, if this woman needed a general anaesthetic for caesarean section? (5 marks)
Question 4
a) How should you manage the perioperative opioid requirements of a patient who is having elective surgery and who takes regular opioids for non-malignant pain? (8 marks)
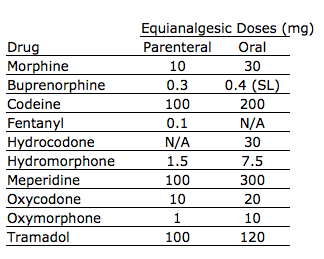
b) Give the conversion factors for oral tramadol, codeine and oxycodone to the equianalgesic oral morphine dose. (3 marks)
c) What are the perioperative implications of an existing spinal cord stimulator? (6 marks)
d) What additional perioperative precautions should be taken if the patient has an intrathecal drug delivery system fitted? (3 marks)
Question 5
a) Which investigations are specifically indicated in the preoperative assessment of a patient presenting for thyroidectomy for treated thyrotoxicosis? (5 marks)
b) What particular issues must the anaesthetist consider during the induction, maintenance and extubation phases of anaesthesia for a
euthyroid patient having a total thyroidectomy? (11 marks)
c) Describe the specific post-operative problems that may be associated with this operation. (4 marks)
Question 6
A 19 year-old patient has suffered a complete transection of the spinal cord at the first thoracic vertebral level due to a fall, but has no other injuries.
a) Outline the sequence of neurological effects that may develop in the first three months following injury. (6 marks)
b) Which disturbances of the cardiovascular, respiratory and gastrointestinal systems may subsequently occur? (8 marks)
c) When and why may suxamethonium be contraindicated in this patient? (2 marks)
d) Give the advantages of a regional anaesthetic technique for a patient having elective lower limb surgery 2 years after a high thoracic spine transection. (4 marks)
Question 7
a) Which specific nerves must be blocked to achieve effective local anaesthesia for shoulder surgery? (6 marks)
b) What are the possible neurological complications of an interscalene block? (6 marks)
c) Outline the measures available to reduce all types of neurological damage during shoulder surgery. (8 marks)
Question 8
a) List the effects of cigarette smoking on the cardiovascular system and on oxygen delivery, outlining the pathophysiological mechanisms involved. (12 marks)
b) List the effects of cigarette smoking on the respiratory system, other than those you have outlined above, that are relevant to the conduct of general anaesthesia. (4 marks)
c) What advice would you give a smoker 24 hours before a scheduled procedure under general anaesthesia and why? (4 marks)
Question 9
a) What are the central and peripheral neurological complications of coronary artery bypass surgery? (7 marks)
b) What are the risk factors for central neurological complications? (6 marks)
c) How can the incidence of central neurological complications be reduced? (7 marks)
Question 10
You are called to the Emergency Department to see a 2 year-old child who presents with a 4-hour history of high temperature and drowsiness. On examination there is prolonged capillary refill time and a non-
blanching rash. A presumptive diagnosis of meningococcal septicaemia is made.
a) What are the normal weight, pulse rate, mean arterial blood pressure and capillary refill time for a child of this age? (4 marks)
b) Define appropriate resuscitation goals for this child (2 marks) and outline the management in the first 15 minutes after presentation. (7
marks)
c) After 15 minutes, the child remains shocked and is unresponsive to fluid. What is the most likely pathophysiological derangement in this child’s circulation (2 marks) and what are the important further
treatment options? (5 marks)
Question 11
A 26 year-old patient with stage 4B Hodgkin’s disease (spread to lymph nodes and other organs) requires an open splenectomy.
a) List the specific factors that are of importance when planning your anaesthetic management. (10 marks)
b)Outline the options for providing postoperative analgesia for this patient and give a possible disadvantage of each. (6 marks)
c) Which vaccinations should this patient receive and what is the optimal timing of these? (4 marks)
Question 12
a) What is meant by the term ventilator associated pneumonia (VAP)? (3 marks)
b) List the factors that increase the risk of the development of VAP. (10 marks)
c) What measures may reduce the risk of development of VAP? (7 marks)
Time to get started on your exam review!
@mb
Examiners’ Report
The SAQ paper is written to contain questions with varying levels of difficulty;
2 questions adjudged to be difficult (pass mark 10-11/20)
8 questions adjudged to be moderately difficult (pass mark 12-13/20)
2 questions adjudged to be easy (pass mark 14/20 or more)
The overall pass rate for this paper was 49.5%
Question 1: CSF Physiology and lumbar puncture
Pass rate 50.9%
This was one of the easy questions in the paper so we would have expected the pass rate to have been a little higher. Some candidates did not answer the question asked in part (d) so lost marks.
Question 2: Dental Sedation
Pass rate 62.1%
This is an important topic and was generally well answered despite some confusion caused by the inclusion of a table that required completion. It had the highest pass rate of all the questions.
Question 3: Pre-eclampsia and severe pre-eclampsia
Pass rate 16.1%
The poor pass rate for this important subject is of concern as pre-eclampsia is a common condition that all candidates should have encountered. Severe pre-eclampsia is an emergency for which the principles of management should be known. Surprisingly few candidates could give an acceptable definition of pre-eclampsia and even fewer knew that control of systolic hypertension is of prime importance in preventing intracerebral bleeding in women with severe pre-eclampsia.
Again, as mentioned above, failure to read the question in part (c) meant that some candidates lost marks by not answering what was asked.
Question 4: Chronic opioid use and analgesia conversion
Pass rate 25.0%
It was anticipated that candidates would find this question difficult and this proved to be the case. Some candidates lost marks because they wrote exclusively about the drugs they would use to manage opioid requirements for this patient but did not mention more general measures such as involvement of the pain team. Very few candidates gave any information about management of transdermal pain patches in the peri-operative period. There are differing opinions as to whether patches should
be continued, particularly in the case of buprenorphine, but candidates were able to gain marks for either opinion provided they showed that they were aware of the potential problems of altered absorption and partial antagonism.
Question 5: Thyroidectomy
Pass rate 31.9%
The first and last parts of this question on pre-operative tests and postoperative considerations were well answered. The majority of the marks were lost in the middle section on issues to be aware of during anaesthesia for elective thyroidectomy. Many of candidates concentrated on management of thyroid storm or difficult airway, both of which are relatively rare during such surgery. It is likely that some candidates failed to read the question correctly because it was clearly stated
that the patient was euthyroid making thyroid storm very unlikely.
Question 6: Spinal injury
Pass rate 49.4%
This question had the highest correlation with overall performance i.e. candidates who did well in this question performed well overall in the SAQ. The examiners commented that part (d) about the advantages of regional anaesthesia for elective lower limb surgery, was not well answered. Candidates tended to give general answers such as “avoids the need for general anaesthesia” or “maintains cardiovascular stability” rather than specific advantages such as “reduces the risk of autonomic dysreflexia” or “avoids postoperative respiratory inadequacy due to
general anaesthesia”.
Question 7: Shoulder block
Pass rate 48.3%
This question also correlated well with overall performance. The anatomy was not well known to a lot of the candidates so quite a few marks were lost here. This is a recurring theme in the Final exam-remember that anatomy relevant to clinical practice is likely to be included. Failure to read the question again caused some candidates to lose marks. Part (b) asked specifically for possible neurological complications of an interscalene block and quite a few candidates wrote about non-neurological complications.
Question 8: Smoking and anaesthesia
Pass rate 55.5%
The relevance of this question to everyday practice makes the fact that it was well answered all the more pleasing. Candidates who lost marks generally did so because they did not know the pathophysiological mechanisms involved in the difficulties caused by smoking. Remember that applied physiology is also part of the syllabus.
Question 9: Neurological complications of coronary artery bypass grafting
Pass rate 54.6%
Candidates who did well in this question tended to do well overall. There was quite a spread of scores with some candidates having a very clear idea of the answers and others seemingly not very much idea at all. Whether this reflects the fact that some candidates sitting the exam have no experience of cardiac anaesthesia is not clear. However, as stated in previous reports, candidates who have no exposure to the mandatory units of training should endeavour to spend a few sessions gaining first hand experience prior to sitting the SAQ paper.
Question 10: Paediatric meningitis
Pass rate 56.9%
The pass rate for this question was the second highest in the paper but the
examiners still felt that it was not particularly well answered. Many candidates lost marks because they wrote similar answers for parts (b) and (c), despite the fact that in part (c) they were asked to comment on what they would do if the measures used in (b) were not successful in resuscitating the child. Incorrect dosages of drugs, particularly antibiotics were often quoted.
Question 11: Splenectomy in a patient with Hodgkin’s lymphoma
Pass rate 38.8%
Many examiners marking this question felt that either the candidates had not read the question as carefully as they should have done, or they lacked knowledge of the implications of Hodgkin’s lymphoma and its treatment for anaesthesia. Rather than focusing on specific factors of importance many ca ndidates wrote about general problems when anaesthetising for a splenectomy. This was reflected in the pass rate.
Question 12: Ventilator associated pneumonia (VAP)
Pass rate 44.3%
This is a common condition that candidates should have seen so it was sur
prising that it was quite poorly answered. Very few candidates were able to give a definition of VAP or to give details of the care bundles used in its prevention and treatment. Merely stating “a care bundle would be used“
suggests inadequate depth of knowledge.
Time to get started on your exam review!
@mb